In cases of severe pelvic injuries, immediate stabilization is often the difference between life and death. While definitive treatments like internal fixation with a pelvis plate can be part of long-term management, emergency care often requires faster, less invasive interventions. This is where external fixation plays a crucial role. For patients with high-energy trauma, such as those from road accidents or falls from significant heights, external fixation helps control bleeding, stabilize fractures, and buy critical time for further medical interventions.
Why Pelvic Fractures Are So Dangerous?
The pelvis is more than just a bony structure; it’s a hub for major blood vessels, organs, and nerves. When fractured, especially in an unstable pattern, it can lead to massive internal bleeding. Many patients with unstable pelvic fractures present with hypovolemic shock, which significantly increases the risk of mortality. In emergency medicine, controlling hemorrhage quickly is the top priority. External fixation helps achieve that by reducing the pelvic volume and stabilizing the fracture site, which in turn limits ongoing bleeding.
External Fixation as a Lifesaving Tool
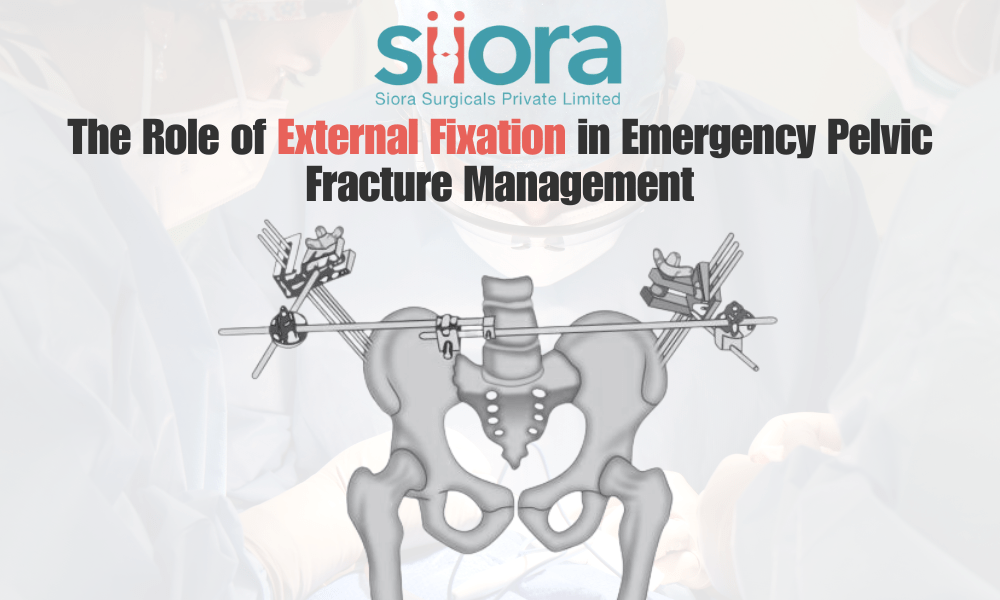
Unlike internal fixation, which involves surgical placement of plates or screws, external fixation is performed percutaneously. Surgeons place pins or screws into the bones through small incisions, then connect them with an external frame. This can often be done quickly in the emergency department or operating room. By realigning and compressing the pelvis, this method reduces bleeding from bone surfaces and torn vessels. It also provides mechanical stability, which is crucial for preventing further soft tissue damage.
For patients who are too unstable to undergo a lengthy procedure, external fixation offers a minimally invasive and rapid solution. It’s not uncommon for trauma teams to use it as a bridge—stabilizing the pelvis first and then moving to more definitive treatments once the patient is stable enough for complex surgery.
Techniques and Considerations
The most common technique for emergency pelvic stabilization is the application of a C-clamp or an anterior external fixator. These devices are relatively quick to apply, often taking less than 30 minutes in experienced hands. The choice between anterior and posterior fixation depends on the fracture pattern, patient anatomy, and available resources.
However, external fixation isn’t without challenges. Improper pin placement can lead to complications like infection or neurovascular injury. That’s why trauma surgeons are trained to perform these procedures under sterile conditions and often with the guidance of imaging tools. The device also needs regular monitoring to prevent loosening or skin complications.
Integration with Other Emergency Measures
External fixation rarely works in isolation. It’s typically part of a comprehensive damage control strategy. Patients with pelvic fractures often need blood transfusions, angiographic embolization to control arterial bleeding, or pelvic packing. In some cases, a combination of external fixation and preperitoneal packing significantly reduces mortality.
Another key aspect is multidisciplinary coordination. Emergency physicians, orthopedic surgeons, interventional radiologists, and critical care teams must work in tandem. The faster this collaboration happens, the better the outcomes for the patient.
From Temporary to Definitive Care
It’s important to note that external fixation is usually a temporary measure. Once the patient is stable, the focus shifts to definitive reconstruction, which may involve internal fixation using plates, screws, or other orthopedic hardware. The transition from temporary to permanent stabilization requires careful planning, as early conversion can improve recovery but must be balanced with the patient’s overall health status.
Final Thoughts
The external fixator has revolutionized emergency pelvic fracture management. By rapidly reducing pelvic volume and stabilizing fractures, it controls bleeding, prevents further injury, and creates a window for life-saving interventions. While it is not the final step in treatment, its role as a bridge in the continuum of care cannot be overstated. For trauma teams, mastering external fixation isn’t just a technical skill; it’s a critical tool in saving lives when every second counts.
Leave a comment